Morton's neuroma is a relatively common but often misunderstood foot condition that can lead to discomfort and pain. This condition can be demystified by exploring essential facts about Morton's neuroma. Morton's neuroma typically occurs between the third and fourth toes, though it can develop in other spaces in the foot. Despite its name, Morton's neuroma is not a tumor. It is actually a thickening of the tissue surrounding the nerves leading to the toes. Common symptoms can include sharp, burning pain or the sensation of a pebble in the shoe, typically while walking or running. Morton’s neuroma can be triggered by wearing tight shoes, high heels, or activities that put repetitive pressure on the forefoot, such as running. Treatment of Morton's neuroma can be managed with conservative measures such as wearing wider shoes, or using cushioned insoles. If conservative treatments do not provide relief, surgical removal of the neuroma may be considered. Effective preventive measures include wearing proper footwear, maintaining a healthy weight, and addressing foot issues promptly. If you have any of these symptoms, it is suggested that you consult a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Kenneth Donovan, DPM of Advanced Care Foot and Ankle. Our doctor will attend to all of your foot care needs and answer any of your related questions.
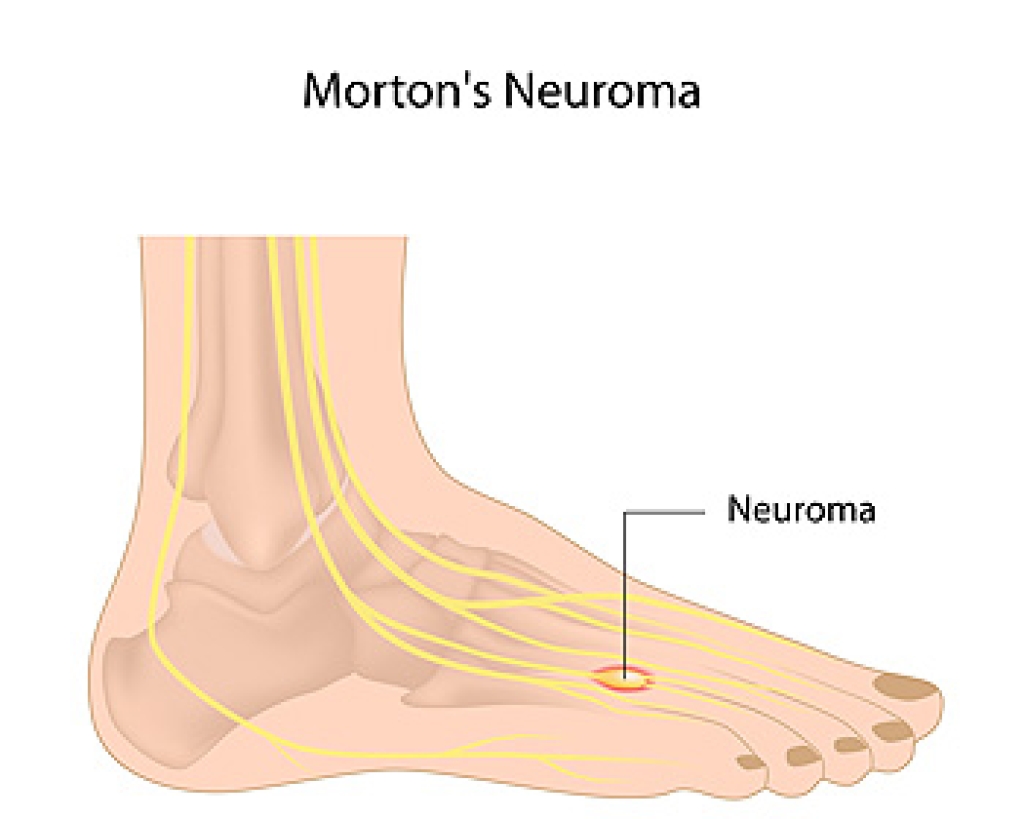
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Charleston, SC . We offer the newest diagnostic and treatment technologies for all your foot care needs.









