Popping ankles refer to the clicking or snapping sounds that occur during movement of the joint. This may happen when tendons or ligaments shift slightly over bone or when gas bubbles form and release within the joint fluid. Causes include repetitive motion, previous injuries, or natural joint structure. Risk factors like weak muscles, loose ligaments, or arthritis can increase the chance of persistent popping and discomfort. While occasional popping may be harmless, frequent or painful episodes should not be ignored. A podiatrist can evaluate ankle function, identify underlying causes, and recommend strengthening and stretching exercises or other treatment options. If popping ankles are affecting your daily activities, it is suggested that you schedule an appointment with a podiatrist to restore comfort and mobility.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Kenneth Donovan, DPM from Advanced Care Foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
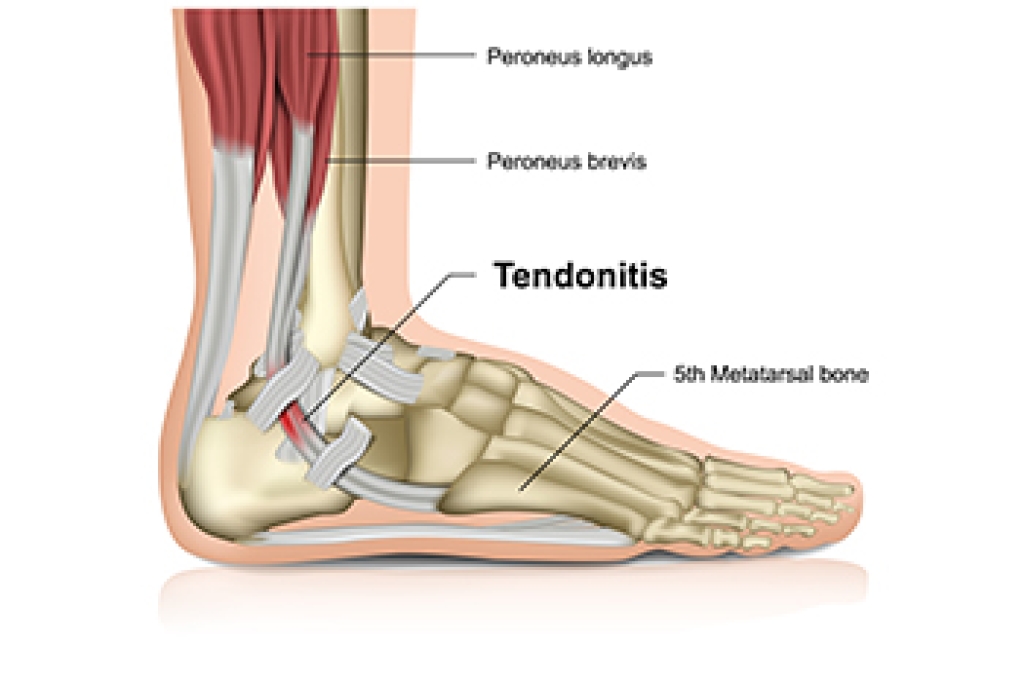
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions please feel free to contact our office located in Charleston, SC . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.